

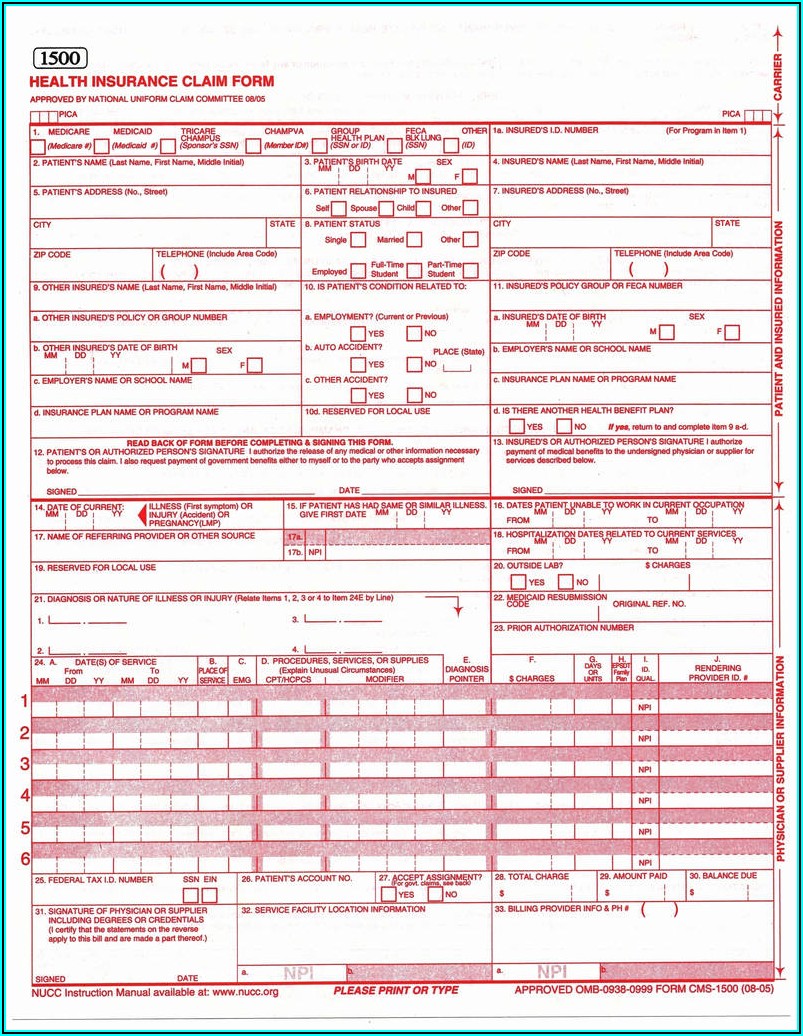
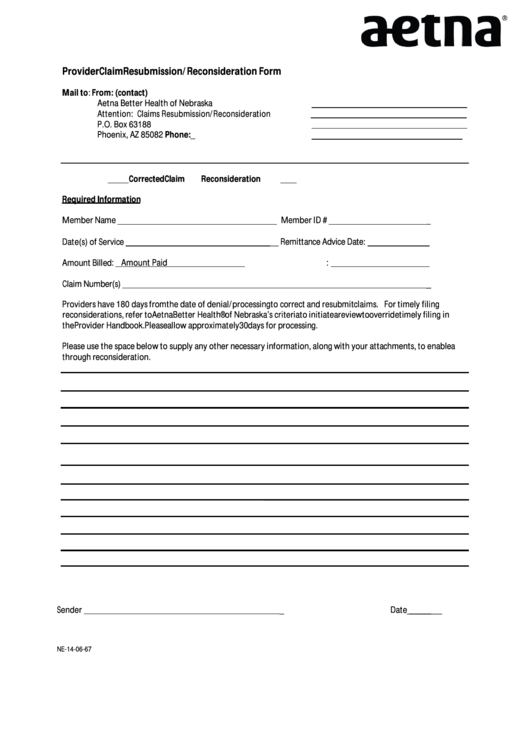
abet in the filing of a fraudulent claim to obtain payment of a. You will receive directions from the Quality Improvement Organization (QIO) regarding additional appeal options. By signing and submitting this form, you certify that the information is true and correct. The Quality Improvement Organization will respond to you as soon as possible, but no later than 14 days after receiving your request for a second review. You may ask for this review immediately, but must ask within 60 days after the day the Quality Improvement Organization said no to your Level 1 Appeal. Within 48 hours the reviewers will tell you their decision. When you'll hear back from the Quality Improvement Organization (QIO) (Please refer to above directions regarding filing an expedited appeal) If you miss the deadline for contacting the Quality Improvement Organization about your appeal, you can make your appeal directly to us instead. You must contact the Quality Improvement Organization to start your appeal no later than noon of the day after you receive the written notice telling you when we will stop covering your care. Additionally, a Level Two report is provided to your vendor, which is the only accepted proof of timely filing for electronic claims. By registering or logging in to your secure site. Electronic submission: Through Electronic Clearing House. You can check claim status: By using Aetna Voice Advantage ® (AVA), our interactive telephone self-service system. You can ask to change this decision so you're able to continue coverage. If a claim is a resubmission or a corrected claim, please send to the above address, Attention: Resubmissions. When your coverage for that care ends, we'll stop paying our share of the cost for your care. You’ll receive a "Notice of Medicare Non-Coverage (NOMNC)" in writing at least 2 days before we decide it’s time to stop covering your care. (Usually, this means you’re getting treatment for an illness or accident, or you're recovering from a major operation.) Claims with TPL (or coordination of benefits) should be submitted within 180 days from primary insurer's EOB date or 180 days from date of service, whichever is later. Corrected claims must be submitted within 365 days from the date of service. Rehabilitation care as an outpatient at a Medicare-approved Comprehensive Outpatient Rehabilitation Facility (CORF). What is Aetna Better Health timely filing limit Timely Filing Requirements of Claims.Skilled nursing care as a patient in a skilled nursing facility Nonparticipating-provider standard timely filing limit change.for electronically submitted claims, provide the second level of acceptance report as proof of timely filing. 108 DISYS 105 HUB International 103 LifeStance Health 101 Charter Global 90 AdTheorent 78 Akkodis 71 Larson Maddox 71 Apex Systems 70 Everest Consultants, Inc.You have the right to keep getting your covered services for as long as the care is needed to diagnose and treat your illness or injury if you’re getting: Untimely Filing of the Claim A review of a claim that was submitted outside the timeframe Provide good cause justification documentation for late filing. 165 The Denzel Group 141 Harbor Freight Tools 140 Mindex 140 Concero 140 Amerit Consulting 138 Optomi 136 UnitedHealth Group 133 Thriveworks 113 Reli.
209 TWO95 International, Inc 175 Net2Source Inc.


 0 kommentar(er)
0 kommentar(er)
